Adult Sepsis for Nurses



Description
This session covers non pregnant adults and children aged 12 years and over. It is aimed at all out of hospital clinicians, GPs, Nurses, Paramedics, Community Midwives and those providing urgent or unscheduled care. It will cover the subtle ways in which sepsis may present and highlight the history, examination and the management of the patient with sepsis. This session has been uptated to reflect the changes in NEWS2 2017 and will be referred to throughout this session.
Learning Objectives
By the end of this session you will be able to:
-
Describe various ways patients with sepsis may present and what to cover in the history
-
List the structured set of observations to support clinical decision making and to help stratify risk
-
Recall common pitfalls in diagnosis
-
Identify which patients with sepsis are highest priority for urgent admission and know about the early management of the patient with sepsis
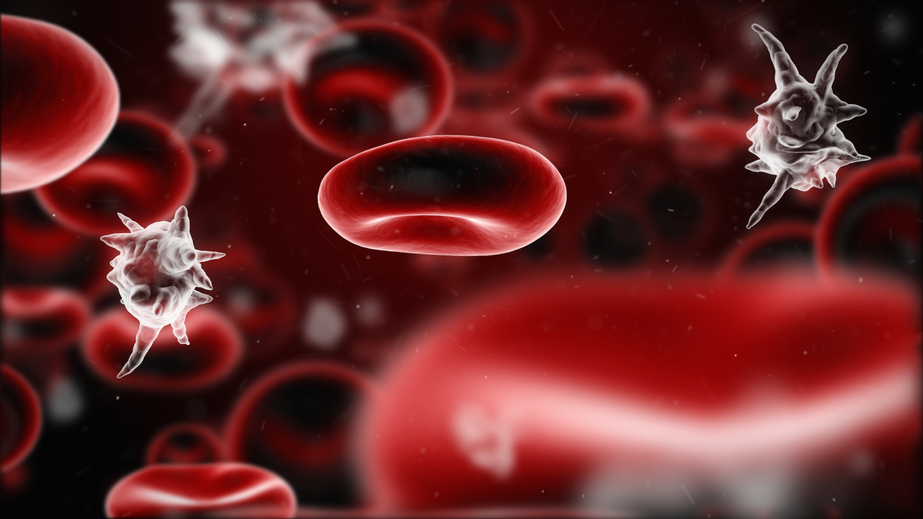
Sepsis is a clinical syndrome when the immune system is switched on in response to infection. This response can be overwhelming and may lead to multi-organ failure.
Sepsis with shock is life threatening as the hypotension does not respond to fluids alone. Signs and symptoms may be very non-specific and can easily be missed especially since people with sepsis may not have an obvious history of infection, and fever is not present in all cases.
Alison Tavaré (MBChB FRCGP MSc DRCOG) is a Bristol GP and the Primary Care clinical lead with the 'Deteriorating Patient' team at the West of England Academic Health Science Network.
As the GP member of the NICE Guidelines Development Group for sepsis, Alison first became involved with the West of England AHSN to raise awareness of sepsis amongst her GP colleagues, but this evolved with the use of NEWS (National Early Warning Scores) to support the identification and management of the sick patient. This work has been a regional and system wide collaboration between primary care, out of hours, the ambulance service, and the acute trusts, and has resulted in a measured reduction from mortality from 'suspicion of sepsis'. The team have won the BMJ Awards 2018 'Patient Safety Team of the Year' and the HSJ 2018 Patient Safety award for the 'Deteriorating Patients and Rapid Response Systems'.
The 'Deteriorating Patient' team are now involved in supporting the national adoption and spread of NEWS2 out of hospital and in addition are working closely with NHSE to develop a regional strategy to improve outcomes for people with learning disability.

- Anaesthesia | Paediatrics | Pharmacokinetic,Pharma...
- Posted By eIntegrity Healthcare e-Learning
- Posted Date: 2024-11-18
- Location:Online
- This session will provide an overview of pharmacokinetic (PK) maturation during infancy and the use of size models to describe PK differences between children and adults. It will go on to describe known pharmacodynamic (PD) differences and consider the im
- Anaesthesia | Paediatrics | Opioids In Paediatrics...
- Posted By eIntegrity Healthcare e-Learning
- Posted Date: 2024-11-18
- Location:Online
- This session looks at practical opioid pharmacology applied to the clinical use of different agents for neonates, infants and small children.
- Anaesthesia | Paediatrics | Advanced Paediatric Li...
- Posted By eIntegrity Healthcare e-Learning
- Posted Date: 2024-11-18
- Location:Online
- This session addresses the advanced management of the critically ill child and the child in cardiac arrest.
- Anaesthesia | Paediatrics | Head Injury
- Posted By eIntegrity Healthcare e-Learning
- Posted Date: 2024-11-18
- Location:Online
- This session describes the principles of stabilisation and management of a child with a head injury and how this differs from the management of an adult patient. This includes methods of assessment, effects and management of raised intracranial pressure,
- Anaesthesia | Paediatrics | Multiply Injured Child...
- Posted By eIntegrity Healthcare e-Learning
- Posted Date: 2024-11-18
- Location:Online
- This session looks at the initial management and stabilization of the multiply injured child with reference to published trauma guidelines.